Accelerating Common and Early-Onset Cancer Detection: We Need Innovative and Equitable Approaches
This blog post is the summary of a talk I gave last week at the Colorectal Cancer Resource and Action Network’s (CCRAN) Early Age Onset Cancers Symposium. I had the privilege of speaking about the potential to advance screening for more common as well as rare tumours in younger adults using innovations in policy and processes. This is what I discussed during my 30 minutes. I want to thank CCRAN as a respected patient advocacy group for bringing this issue to light every year!!
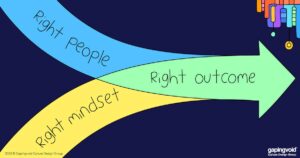
In recent years, we have observed a concerning rise in early-onset cancers among younger adults, both common ones where you least expect them, and rare and serious types which catch everyone by surprise. For many of these patients, the path to a timely diagnosis remains challenging and fraught with barriers. As a family physician and a healthcare policy advocate, I believe we urgently need to evolve our cancer screening practices to better meet the needs of these younger populations. Our approach should center on precision, accessibility, and the empowerment of both patients and healthcare providers. Here, I explore the key areas where innovation and policy shifts could make a difference.
- The Distinction Between Screening and Diagnostic Pathways
Screening for cancer is typically applied to a healthy population with no symptoms, aiming to detect disease signals before clinical presentation. However, when symptoms arise, patients move into diagnostic pathways, which are often more complex and vary widely based on the type of cancer and available resources. Unfortunately, younger adults presenting with symptoms often encounter skepticism or delays in diagnosis due to their low statistical likelihood of having these serious conditions. This disconnect between statistical probability and individual presentation can lead to patients feeling dismissed, a concern raised frequently by young adults navigating healthcare for rare cancers.
To bridge this gap, we need to strengthen diagnostic pathways for symptom-based presentations, particularly for younger adults. Standardizing and centralizing these pathways could offer more streamlined, equitable access to diagnostics for rare cancers in this demographic.
Addressing Inconsistencies and the Role of Guidelines
Cancer screening protocols are largely governed by guidelines, which vary across provinces and regions due to differences in funding, equipment availability, and healthcare workforce capacity. While these guidelines aim to balance safety, effectiveness, and resource allocation, they often lack consistency. For example, breast cancer screening age cut-offs differ across provinces, creating confusion and potential delays in diagnosis, especially for mobile populations. Nationally consistent cancer screening parameters could address these disparities and help equalize access to critical screenings. Such standardization would ensure that no matter where a young adult lives, they receive the same access to disease detection.
Moving Toward Centralized and Automated Screening Systems
Screening large, healthy populations for early signs of common cancers is best managed through automated, centralized programs. By centralizing processes, we can reduce the workload on individual clinicians and ensure that high-risk patients are not overlooked. Centralized systems with automated callback programs—reminders to complete a screening or follow up on results—and even care navigators to book appointments, could significantly enhance continuity of care and improve participation rates. Some provinces have these programs (such as the Cancer Care Ontario’s population approach), but citizens still need to exert real energy to get the tests they need. Every step where a decision to act or not act means our rates may decrease, especially with equity deserving populations.
Automation can further support healthcare professionals who may not have the bandwidth to individually assess every patient’s risk profile. AI-driven tools are essential for identifying high-risk individuals at scale, allowing practices and regional networks to prioritize these patients for screening. These tools rely on large data bases to be mined and scanned, and these are becoming more available by our Ministries of Health as they consolidate data assets.
 Prioritizing Equity and Accessibility in Patient Education
Prioritizing Equity and Accessibility in Patient Education
Equity and accessibility should be at the core of any screening program. For many communities, particularly underserved and marginalized populations, traditional patient education materials may not be enough to encourage engagement with screening programs. We need to ensure that these materials are culturally sensitive, accessible in multiple languages, and available in non-traditional formats that resonate with diverse communities.
Accessible education is not merely a matter of providing information; it involves creating trust and building awareness within communities where cancer screening rates may be lower (underscreened or never screened groups and individuals). By investing in community or population centred approaches to patient education and outreach, we can foster greater acceptance of cancer screening services and increase early detection rates.
Harnessing AI for Routine Disease Detection, and Targeted Screening for Unusual Diseases
AI has significant potential to transform cancer screening, but it faces limitations due to current data constraints. The vast datasets required to recognize rare cancers, genetic predispositions, and aggregate risk factors often remain siloed or incomplete. Expanding AI capabilities necessitates integrating larger, more diverse datasets, including genetic and epigenetic information, to enable more precise risk assessments and better identify high-risk individuals. With this comes significant concerns about privacy and security. As well, we may have to consider consent, even if information is collected via legislated means, simply because it is the right thing to do. But, even this can be automated.
If we approach the above policy issues with a view to solutions, AI also opens the door for personalized screening algorithms that cater to individual risk profiles rather than blanket population-level screening. This is where the real potential lies in detecting early age onset cancers. For example, a young adult with a family history of rare cancers could receive tailored screening protocols, taking into account specific genetic markers or lifestyle factors. Signals detected in genetic information matched against known diseases will find people who do not fit into evidence based guidelines at the population level. Their screening can be individualized and tailored. Such personalized approaches would be invaluable in identifying rare and early cancers, especially those with low overall likelihood but high personal risk.
Emerging technologies, such as circulating tumor DNA (ctDNA) blood-based tests, offer promising alternatives to invasive procedures. These minimally invasive tests could provide diagnostic insights for patients in remote or underserved areas, making it possible to reach populations with limited access to specialized facilities or equipment like mammogram or MRI machines. Genetic panels and advanced epigenetic analyses are also on the horizon and gaining evidecne, holding the potential to further individualize cancer risk assessments.
 Policy Support for Equitable, Future-Ready Screening Programs
Policy Support for Equitable, Future-Ready Screening Programs
For these changes to be sustainable, policy support is crucial. Healthcare policies must prioritize equitable access to screening and diagnostics across all provinces, ensuring that young adults, particularly those from underserved areas, have access to timely and effective cancer screening when they need it. Supporting research into novel screening methods and AI-based algorithms should also be a priority, fostering an environment where healthcare can evolve with the needs of the population as a group, but also as a series of individuals.
Policy initiatives must also address discrepancies in healthcare workforce allocation, as some provinces face greater staffing shortages than others. Some serious national consideration must be given to seeing now tests can come to patients, rather than patients to the tests. As well, where testing can be simplified and the processes for accessing them made one step easier (over and over again), we will see rates rise to levels that we may never have seen before.
Conclusion
The rise in early-onset cancers demands a proactive, innovative response. By combining centralized screening programs, culturally sensitive patient education, AI-driven analytics, and equitable policy initiatives, we can better support younger adults facing the challenges of rare and serious cancers. Early detection is critical, but it must be accessible, personalized, and responsive to the unique needs of this group. Our responsibility as healthcare providers and system leaders is to ensure that no patient feels dismissed or overlooked due to age or rarity of disease in a population. Through a comprehensive, future-focused approach, we can transform cancer screening and diagnostics to meet the challenges of our evolving healthcare landscape, increasing rates of early detection and thus hopefully successful treatment.


2 Replies to “Accelerating Common and Early-Onset Cancer Detection: We Need Innovative and Equitable Approaches”
“The future is already here, it’s just not evenly distributed.”
Osler healthcare system using liquid biopsies in Ontario: https://www.williamoslerhs.ca/en/news/osler-leads-the-way-as-first-in-canada-to-offer-life-changing-precision-cancer-care-technology.aspx
This is great to hear Charles! And yes, equity is an issue here. And price. And selectivity… the right test for the right person for the right disease. We have to figure how to move from diagnosis to appropriate screening in this space.
Thanks for commenting, as always!!