The Future of Primary Care in Canada: Collaboration in Care and Policy
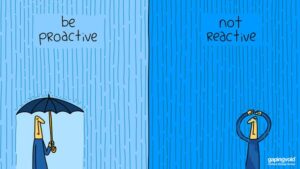
Welcome to the final part of this four-part series on trends in primary care in Canada. In this installment, we cast our gaze into the future of healthcare, exploring high-level concepts that are set to transform primary care delivery, and which we must face head-on. Collaboration between clinicians and policymakers will be key to ushering in these changes and ensuring that healthcare in Canada remains patient-centric and effective. Let’s delve into some high-level concepts that will shape the future of primary care now and in the near future.
Telemedicine and Advanced Technology:
Clinicians: Embrace advanced telemedicine and telehealth technologies to provide efficient care. Telemedicine will become an integral part of primary care, offering convenient access to healthcare services.
Policymakers: Foster an environment that supports continued telehealth innovation while ensuring quality, access, and data security. Encourage investment in broadband infrastructure for equitable telehealth access, ensuring no one is left behind.
AI, Genomics, and Precision Medicine:
Clinicians: Prepare for AI-driven decision support and personalized treatments. AI and genomics will revolutionize diagnostics and treatment, offering tailored solutions for individual patients. This is new to us. We must learn how it impacts decision-making and trust.
Policymakers: Invest in AI research and ensure regulations accommodate AI-driven diagnostics and genomic medicine. Promote data sharing while protecting patient privacy, striking a delicate balance. Ensure that AI tools are properly trained on data that reflects our society and values. Regulate where necessary but not to the point of stopping innovation.=
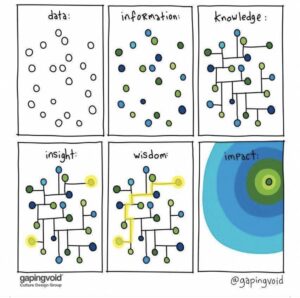
Health Data Ownership and Privacy:
Clinicians: Advocate for patients’ data control and privacy rights. Patients should have a say in how their health data is used and shared. Practice these rules and uphold them in your practice. Patients will benefit from full access to their records all the time, in real-time. This has been proven over and over in large studies. EMRs should become fully open to them, including the ability to enter data directly to the record.
Policymakers: Develop robust data ownership policies that balance patient rights with the need for data sharing for research and care coordination. Privacy and data security should be at the forefront of healthcare data management. Clinicians should not be solely responsible for data stewardship and custodianship. Benefits are shared thus risks must be shared. Those who produce data must be incented to share it. This is net new work for most doctors.
Technological Advancements:
Clinicians: Stay informed about emerging technologies and consider how they might enhance your practice. Breakthroughs like Virtual Reality (VR) and Augmented Reality (AR) tools have the potential to enhance patient care and medical training. There are products available now that let you learn, train and share with others.
Policymakers: Support research and development of healthcare applications for VR and AR and establish guidelines for their responsible use in patient care. Vet products for safety, accuracy and clinical application. Make it easier for clinicians to adopt new technology by getting policy blockers out of the way.

Rural and Underserved Area Demands:
Clinicians: Consider working in underserved regions utilizing telehealth to reach remote populations, addressing healthcare disparities. Consider how your skills may be well used beyond the walls of your clinic to fill gaps in regions or zones of high need. Train your residents to have skills that instill confidence in their ability to serve rurally.
Policymakers: Implement policies that incentivize healthcare professionals to serve in rural areas and expand telehealth infrastructure in underserved communities, ensuring equal access to care. Forcing physicians out of the cities in punishment, not incentive. Collaboration with telemedicine companies and creative thinking around areas like licensing are required.
Environmental Health:
Clinicians: Be aware of environmental health impacts on patients and incorporate this knowledge into preventive care. Consider how your practice can be greener and reduce waste.
Policymakers: Develop policies addressing environmental health concerns and promote sustainable practices in healthcare, recognizing the interconnectedness of health and the environment. Create climate-friendly systems that reduce waste and consumption.
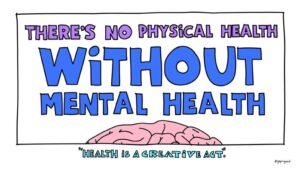
Mental Health Integration:
Clinicians: Collaborate with mental health professionals and stay attuned to mental health needs as mental health takes a more prominent role in overall health. Bring truly team-based care into mental health domains.
Policymakers: Promote policies that integrate mental health into primary care, improve access to mental health services, and address the mental health workforce shortage, recognizing its importance in holistic care. Fund providers other than physicians and hospitals for mental healthcare delivery. Make this a population priority.
Global Health Views:
Clinicians: Be prepared for your role in pandemic response and public health emergencies, as primary care plays a crucial role in global health crises. We musts not forget the lessons of COVID-19 and must stay vigilant at all times.
Policymakers: Invest in public health infrastructure and preparedness, ensuring primary care’s central role in global health crises and fostering international collaboration. This cannot be an afterthought and cannot be the brunt of endless cutbacks. Remember, the next pandemic could be tomorrow.
Alternative Payment Models and Workforce Adaptation:
Clinicians: Embrace new payment models and adapt to evolving roles in the healthcare system. Embrace teams. Consider how others may be tasked to do things that you have always done and bring your training to bear in comprehensiveness, complexity and oversight. Disentangle your work flows from old fee-for-service thinking.
Policymakers: Continue payment reform efforts, incentivizing value-based care, and invest in healthcare workforce development to meet changing demands and ensure high-quality care for all Canadians. Work with clinicians to ensure that the right person delivers the right care at the right time and that appropriate funding follows. Consider how private payors like insures and patients might supplement what public funding does not. Create partnerships with corporate entities that enhance what doctors do.
The future of primary care in Canada is brimming with opportunities and challenges. It will require the collective efforts of clinicians, policymakers, citizens to navigate these changes successfully. Collaboration and innovation will be essential to building a healthcare system that is patient-centric, technologically advanced, and responsive to the evolving needs of the population. Together, we can shape a brighter and healthier future for healthcare in Canada.
I welcome your critical thoughts, comments and additions! Please add them to the conversation!!

