Unraveling the Potential of AI in the Medical Practice: What Tools are There?

We have talked a lot about the issues surrounding AI in our medical practices, but now it’s time to think about tools we can use to improve our work lives. Several types of AI applications have the potential to be integrated into office settings now or very soon, offering benefits to both healthcare providers and patients. These AI tools can assist doctors in delivering more efficient, accurate, and patient-centric care. This assumes that the AI products have good data from an EMR to act upon, knowledge of the best evidence, and perhaps even some sense of what patients want. Here are some examples of tools that are here or with us very soon:
Clinical Decision Support Systems (CDSS):
CDSS can provide doctors with evidence-based recommendations and guidelines at the point of care. These systems can assist in diagnosing diseases, suggesting treatment options, and identifying potential drug interactions or allergies. They use data about your patient and compare it to guidelines and best practices to help you make confident decisions. This is becoming more and more automated. There is great potential in alerting us of issues we may have glanced over or missed.
Remote Patient Monitoring:
AI-powered remote monitoring devices can track patients’ vital signs and health metrics in real time. Primary care providers can use this data to manage chronic conditions and intervene when necessary proactively. Intelligent alerts are possible. We do not need to know every 100,000 heartbeats in a day, but we need to know when a patient is in A Fib, for example. AI rules can curate and make sense of masses of information in as it is being produced.
Natural Language Processing (NLP):
NLP tools can help doctors extract valuable information from unstructured clinical notes, medical records, and patient histories. This can save time and improve data-driven decision-making. Data can be coded in whatever coding system is preferred, extracted, transferred, normalized, anonymized and even shared to other systems more effectively with NLPs. Computers like coded data. NLP products can code our words for us and allow better mapping to other systems if we choose or are mandated to share it.
Healthcare Chatbots and Virtual Assistants:
Chatbots and virtual assistants can handle routine administrative tasks and appointment scheduling and provide patients with information about their conditions and treatment plans, freeing up doctors’ time and their staff. Some avatar-based assistants take emotional context into account and read facial expressions! These can be the front door to our clinics and ensure that patients are answered quickly and moved to the right care provider efficiently.
Disease Risk Prediction:
AI models can analyze patient data to predict the risk of developing certain diseases or conditions. Primary care providers can use these predictions for early intervention and prevention strategies. Health systems already use products built in Canada to monitor and report local disease outbreaks very early on!
Medication Management:
AI tools can assist in medication management more than identifying potential interactions. They can adjust dosage and remind patients to take their medications as prescribed. They can even be used to track adherence to a complex treatment regime over time and make comments about treatment success. This analysis can be used to prompt behaviour change in those who are trying hard to do the right thing for their illness.
Patient Triage:
AI-driven triage systems can help prioritize patients based on the severity of their symptoms or conditions, ensuring that those needing immediate attention receive it promptly. Very exciting developments are helping patients decide the right type of visit with the right person for the right problem.
Personalized Treatment Plans:
AI can analyze patient data to create personalized treatment plans, accounting for individual factors such as genetics, lifestyle, and medical history. This can bring us closer to Personalized medicine that seems less rote and formulaic. Evidence can be applied alongside patient preference and plans for best care created in real-time, then curated over time as information changes.
Telehealth and Telemedicine:
AI-enhanced telehealth platforms can facilitate remote consultations, allowing patients to connect with primary care providers virtually. AI can assist in diagnosing and triaging patients during these virtual visits. They can search for language, mood, facial expression and history cues that might help a new clinician make better decisions with a patient. Even conversations and text chains can be analyzed for cues of risk or harm, with patient consent to participate.
Administrative Efficiency:
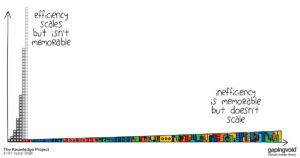
AI can streamline administrative tasks such as appointment scheduling, billing, and insurance processing, allowing primary care providers to focus more on patient care. You will see a whole host of companies offering automation tools for practices that take much pedantic administrative work out of the hands of people who don’t like it and let it be run by machine. This will allow our staff to focus on more important human-centric tasks. Automation is way behind in healthcare. We are getting there, though!
The successful adoption of AI tools in community practices will depend on addressing some healthcare professionals’ concerns and distrust. This can be achieved through education, training, transparent AI development, and ongoing collaboration between healthcare providers and AI developers. As AI technology continues to mature and demonstrate its value in improving healthcare outcomes, its integration into primary and specialist care in the community will be more evident. Our practices will look very different in 5 years!
Stay tuned for Part 6: How do we train the beast? An endless feeding on data.
Hit subscribe to have these delivered right to your inbox!