The Shifting Landscape of Primary Care in Canada – Physician Perspective
This is the second post in a four-part series on my blog, about current trends in Primary Care in Canada. These trends are not all encompassing, but I think they serve as a great starting point for discussion around what is needed to properly transform health care delivery in the community, making Family Medicine a thriving and sought-after field. As usual, the point of my writing is not to prove a point, but in fact to create discourse. I truly welcome your thoughts, other ideas and dissenting opinions! This is what produces impact and changes conversations. So here we go!!
Primary care physicians in Canada are experiencing a period of significant transformation and adaptation. As they navigate the changing healthcare landscape, several trends are emerging that shape their roles, challenges, and aspirations. Let’s delve into these physician trends in primary care and understand how they are impacting healthcare delivery in the country.
- Aging in Tandem with Patients:
Primary care physicians are aging alongside their patient population, leading to human resource-related challenges. As older physicians consider retirement, there’s a pressing need to recruit and train new healthcare professionals to fill the gap and ensure continued access to care for patients. The problem is, physicians are leaving or changing practice at a faster rate than we can create now ones.
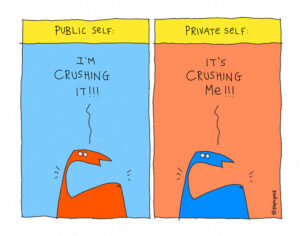
- Burnout and Scaling Back:
Physicians are increasingly reporting burnout symptoms and a tendency to scale back their workload. The demanding nature of primary care, coupled with administrative burdens, is taking a toll on their well-being and productivity. This has many ripple effects across the system, from patient satisfaction to policy planning.
- Overwhelmed by Gatekeeping Responsibilities:
Primary care physicians often find themselves overwhelmed by a multitude of responsibilities, from paperwork and task delegation to ensuring service accessibility and patient advocacy. The increasing complexity of healthcare, combined with limited resources, adds to their stress. During times of system stress, there is also tremendous downloading onto the backs of family physicians from specialists, hospitals and regional services. The load of carrying a practice simply gets heavier and heavier.
- Mental Health Burden:
Physicians are grappling with a rising mental health burden among patients, but acquiring suitable evaluations and care can be challenging. Many mental health services are mostly uninsured and expensive for patients, making it difficult to provide comprehensive mental healthcare. As well, in much of our country mental health care workers are spread very thinly, if they exist at all. Wait times are incredibly long and access is very difficult. Sadly, technology has not filled many gaps here.
- Outdated Digital Systems:
Physicians are experiencing fatigue from outdated digital and electronic systems in healthcare. Subpar and disjointed systems with minimal innovation often require self-funding for upgrades. This hinders efficient data sharing and communication between healthcare providers. Incentives for sharing of data for larger health system use are generally non-existent or completely misaligned. Add to this that governments do not have a high level of trust with doctors’ technology partners, like EMR companies. And the reverse is also true. We are at an impasse here.
- Embracing New Technologies:
To alleviate some of the digital challenges, physicians are exploring newer technologies like ambient note-takers, digital scribes, and back-office automation bots to streamline administrative tasks and improve overall efficiency. There is fatigue and distrust in embracing these technologies fully though, and they are expensive, with no system support for funding. Even though there may be an ROI for these systems, often this is a long way off and difficult for doctors to appreciate.
- Financial Pressures:
Medical inflation is outpacing schedule of benefits fee increases, leading to cost-cutting measures that can impact the delivery of care. Physicians may face difficult decisions regarding resource allocation, particularly with the staff they choose to hire. As well, in most provinces negotiations on fees with government are limited by four-year contracts, political cycles, and for many doctors, poor representation of their specialty area.
- Changing Physician Profile:
Recent graduates differ significantly from those trained over 20 years ago. They are more inclined towards team-based care, and true team-based care is actually hard to find! There is a much higher representation of women in primary care, and this has been a boon to the profession in so many ways, but their professional needs are often not the same as men trained two decades earlier. Younger female and male physicians are now prioritizing work-life balance, seeking diverse roles, and are shying away from solo practice. Newly trained physicians have learned from our past mistakes as a profession and are setting boundaries. Many family medicine graduates are choosing not to go into a traditional comprehensive care practice at all. They are choosing more predictable work as hospitalists, primary care consultants and consultants. An increasing number of residency graduates are even opting never to practice at all! This is not uncommon in other professions like law and engineering, but it is new to medicine. We have to look ahead 10 years and take these changes into account.
- Extending Family Medicine Training:
There is a trend and push toward extending family medicine training to a standard three year residency, with a rise in primary care sub-specialties accredited by the College of Family Physicians of Canada (CFPC). The need for this is a hotly debated topic. Comprehensive generalist care is becoming less appealing to new graduates. This is happening at a time when what our citizens need is greater access to comprehensive thinking and care delivery. So, things may get much worse before they get better.
- Shift Towards Salaried Positions:
Less than a decade ago senior physician leaders were pilloried over their views on moving from fee for service reimbursement to salaried or performance-based pay. Newer physicians are more likely to seek salaried positions or well-defined contracts rather than engaging in the small business aspects of private practice. Smaller physician practices are becoming unsustainable, leading to the rise of multidisciplinary associations, sometimes funded by private entities.
- Growing Demand for Alternative Primary Care Providers:
There is a growing demand for other primary care providers, such as nurse practitioners and physician assistants, to complement physicians. Proper funding is essential to support these providers, who can extend access to care. They are also currently not being trained in sufficient numbers to meet the demand, and need learning in how to operate effect teams, just as doctors do.
- Patient-Centered Approach:
Physicians are trying hard to emphasize a patient-centered approach, shared decision-making, and personalized care plans. However, existing incentives within the healthcare system usually do not align with these goals. Providers are disincentivized to take time with individual patients, even though time with them is a basic requirement for building trust. During times of stress and retraction “customer service” is much harder to achieve, eroding trust even further.
- Addressing Health Inequities:
Physicians are increasingly aware of health inequities and the social determinants of health. They face these with their patients every day. However, their capacity to address these complex issues is limited within the current healthcare system. It requires multilayered health system support. Lack of that leads to despondence and hopelessness in our care provider community. This erodes the sacred physician / patient relationship we hold dearly.
As I have described, primary care physicians in Canada are facing a dynamic landscape characterized by demographic shifts, technological challenges, and evolving healthcare practices. As the healthcare system continues to transform, it’s crucial to support healthcare professionals in their efforts to provide high-quality, patient-centered care while addressing the challenges they face. This includes recognizing the need for recruitment, training, and innovative solutions to improve both physician well-being and patient outcomes. Physicians need it. Patients want it. And the health care system will benefit from it in the long term.
Part three of this series, coming at the start of next week, will contemplate what is happening at the health system level. Stay tuned! I truly welcome your input and comments. Thanks for reading and sharing!

